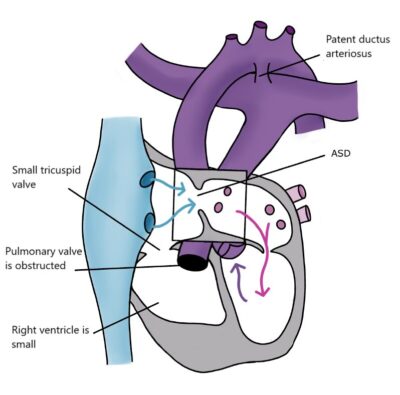
Pulmonary atresia with intact ventricular septum, PA+IVS
In Pulmonary Atresia with Intact Ventricular Septum (PA+IVS), there is no direct connection between the heart and the pulmonary artery. Blood flows to the lungs via the ductus arteriosus. The right ventricle may be very small (hypoplastic) or very large if there is significant regurgitation at the tricuspid valve.
After birth, the child is given continuous intravenous medication to prevent the closure of the ductus arteriosus until heart surgery can be performed. The child urgently needs a shunt to ensure blood flow to the pulmonary artery. Further treatment depends on the structure of the pulmonary vasculature, the functionality of the atrioventricular valve, and the performance of the left ventricle. Sometimes the pumping efficiency of the left ventricle is reduced due to additional openings (fistulas) and narrowings in the coronary arteries often associated with PA+IVS.
If the coronary arteries and left ventricle function well, pulmonary circulation is well developed, and the atrioventricular valve is intact, it is possible to perform a so-called single-ventricle repair (UVH). In this surgery, the superior vena cava is connected to the pulmonary artery at around six months of age (the bidirectional Glenn procedure), and the inferior vena cava is connected to the pulmonary artery at around 3–4 years of age (the TCPC procedure). After this surgery, low-oxygen venous blood flows directly to the pulmonary artery under venous pressure, and the left ventricle acts as the sole ventricle, pumping oxygen-rich blood from the lungs through the aorta to the entire body. This heart defect cannot be completely repaired, and patients require lifelong cardiac monitoring.